

IMPOTANCY
Impotency is the main difficulty amongst 1 people in the 3 and there are two sort of impotency. You can call erectile dysfunction also in this condition guys are not satisfy their partner who males doing masturbation quite badly mostly individuals who suffered with this difficulty but this difficulty is the two variety in the male Initial Males with primary inability have never ever had satisfactory erection for fulfilling intercourse. This form of impotence is uncommon and is habitually brought on by tremendous psychological situations, such as intense worry of familiarity extreme feelings of guilt, and extreme anxiousness. Second men are that defined as the loss of erectile function right after a period of standard function, is far more typical. Guys with secondary erection are typically able to engage in intercourse only 25% of the time. This form of erection usually comes on gradually and is usually a lot more effortlessly treated that principal impotence
There are men’s who mainly having complain for ED1. Diabetes2. Kidney disease3. High blood pressure4. Depression5. High cholesterol6. Any type of pelvic surgery7. Spinal cord or nervous system disorders8. Far more Smoking & drinking
Many individuals who do not have sex want or his lifestyle partner also symptoms of impotency
How To Care By Diet plan-
Diet is the significant reality for any kind of well being but in the erectile dysfunction is a main concern and due to the fact several folks obtaining shame to clarify this issue and really feel a hesitation to consult with medical doctor. Suitable taking diet can get improvement in this ED problem taking a 6 bananas in the morning and chewing it till it not melt like a gum then take 1 glass of milk immediately after it and take a Elvira oil half spoon and Half spoon of kalonji oil taking it with mix each take in ahead of break fast and then after 1 hour get bananas With milk. And keep away from oily & spicy food oil mound must also used for massage on your penis these are the house remedies. Garlic also excellent in case of loss of sexual power due to any of the perform 2-three cloves a of fresh peeled garlic just chew everyday on an empty stomach. if you just tiny crush the cloves and leave for 5-10 minutes in the air for oxidation, it may possibly be more effective as the active ingredient in garlic allicin and far more offered you can also use garlic liberally, although preparing food for diet program.And there are lot product in the market on the medical shop for avoiding erectile dysfunction not only medicine but also lot of ailment offered must take in the prescription of medical doctor and favor only herbal product.
What is erectile dysfunction (ED)?
Impotence, or erectile dysfunction, is the inability to achieve an erection, and/or dissatisfaction with the size, rigidity, and/or duration of erections. According to the National Institutes of Health (NIH), erectile dysfunction affects up to 30 million men.
Although in the past it was commonly believed to be due to psychological problems, it is now known that for most men erectile dysfunction is caused by physical problems, usually related to the blood supply of the penis. Many advances have occurred in both diagnosis and treatment of erectile dysfunction.
What are the risk factors for erectile dysfunction?
According to the NIH, erectile dysfunction is also a symptom that accompanies many disorders and diseases.
Direct risk factors for erectile dysfunction may include the following:
Age appears to be a strong indirect risk factor in that it is associated with increased likelihood of direct risk factors, some of which are listed above.
It is estimated that about 4 percent of men in their fifties, and nearly 17 percent of men in their sixties, have difficulty achieving an erection. Accurate risk factor identification and characterization are essential for prevention or treatment of erectile dysfunction.

when a man reaches middle-age and
beyond gradual changes in his ability to function sexually will
occur. Older men often notice reduced libido, a lessening in their
ability to sustain an erection and a reduction in their ability to
sustain a sexual encounter. Symptoms such as these are common but
not necessarily universal. However, they can also impact on the
fertility of a man. These symptoms can be preceded or accompanied
by associated urinary problems.
Some men will not experience any
reduction in urinary functions or sexual power and prowess.
However, the vast majority of men will have to deal with at least
some of the above issues as they get older.
Testosterone is the male hormone
circulating through a man’s body that is responsible for the
development and maintenance of the male organs and characteristics
such as facial hair, muscle mass and body hair. It is also
responsible for the growth at puberty of the prostate gland, penis
and testicles. Post-puberty it is also responsible for the
production of sperm by the testes. Testosterone is also important
in a male for regulating moods and the libido. Hence, the level of
testosterone in a man’s blood can affect his fertility. The level
of testosterone in the blood is maintained by a feed-back mechanism
starting in the brains hypothalamus.
An important part of this mechanism is
as follows; the hypothalamus stimulates the pituitary gland (also
in the brain) to produce and release the hormone LH (luteinizing
hormone). LH stimulates the Leydig cells in the testicles to
produce and release testosterone. Unfortunately the Leydig cells do
not release the hormone testosterone uniformly throughout any one
24 hour period. Instead the release of testosterone is rather
spasmodic.
Generally the levels of
testosterone in a male’s blood will vary in line with other
functions of his general circadian rhythm. eg Alertness, metabolism
and the release of other hormones. Generally these are at their
peak during the morning and decline as the day goes on. Considering
the role of the hormone testosterone in the male, this may well
explain why some men experience a level of sexual arousal in the
morning greater than that in the evening. The circadian rhythm can
also have an effect throughout the year. Contrary to popular
belief, generally levels of testosterone in males are higher in the
fall than in the spring when …. allegedly …. “a young man’s fancy
turns to thoughts of love”.
Any time from the age of around 40
years the testosterone level in a man can start to diminish. The
main causes of this are that the pituitary gland gradually secretes
less of the hormone LH. This leads to a reduction in the level of
stimulation to the Leydig cells and hence a drop in the production
and, therefore, the release of the male hormone
testosterone.
The result of this is that there is a
slow but sure reduction in the male libido, arousal and the quality
of his erection. By the age of 50 years 1 in 5 males (20%) can
experience erections inadequate for sexual penetration. At age 60
years the figure rises to 30% (3 in 10) and by the age of 80 years
it is 50% (1 in 2). This does, of course, also mean that
approximately 80% of men at age 50 experience no such sexual
problems.
However, as previously mentioned, the
production of testosterone is essential to the production of sperm
– the male gamete. Therefore, as the level of testosterone falls it
will lead to a decline in the ability of a male to father
children. Advancing years do not inevitably lead to male
infertility, after all 1 in 2 octogenarians are still capable of
fathering a child.
According to the World Health
Organization (WHO) there are an estimated 60-80 million infertile
couples in the world. Earlier, it was believed that not being
able to conceive was due to ‘female problems’. It is now recognized
that a couple’s infertility could be due to disorders in the female
reproductive system, the male’s reproductive tract or in
both.
It is estimated that infertility
is:
• solely due to the female in
around 40% of the cases;
• around 30% is due solely to
male factors; and
• 30% is due to a combination of
both partners having abnormalities in their reproductive
systems.
Infertility in women can be treated more successfully than in men. If a couple having normal, unprotected sex have been unsuccessful in conceiving for over a year, then it is important for both partners to get themselves tested for infertility. Studies show that approximately 50% of infertility cases are related to male infertility factors. If you are concerned about your fertility, it is a good idea to get in touch with your health provider and get yourself investigated for possible infertility.
So, what does testing for male infertility entail?
1. Medical History: Your
health provider will require your medical history which will
normally include details about your age, your sexual and
birth control practices, medications you are taking or have
been taking, your use of caffeine, tobacco, alcohol or drugs like
marijuana etc., your exercise patterns and any history of
sexually transmitted diseases.
2. Comprehensive Physical
Examination: A physical examination will be conducted to
assess your overall health and to check for any obvious signs of
infertility which will probably include a testicular
examination.
3. Semen Analysis: A simple
procedure, you will be required to collect your sperm in a specimen
jar for testing. The semen will be analyzed to check for
volume of ejaculate, appearance, sperm count, motility and
morphology, all of which have a bearing on male
fertility.
Depending upon the results of the above tests, you may be required to undergo further investigations that could include blood or urine tests.
• Blood samples will be taken
to test levels of testosterone and Luteineizing Hormone (LH – which
indicates if there is a problem in the pituitary
gland).
• Urine samples would be required
to check if there are any signs of sexually transmitted disease or
for the presence of sperm pointing to retrograde ejaculation (where
the ejaculate flows back into the bladder).
If your health provider thinks that it is necessary to conduct further investigations, they will most probably include the following:
a) Vasography: An x-ray
test that determines if there is a leakage or blockage of sperm in
the vans deferens.
b) Ultrasonography: A test
employed to locate the presence of a blockage or damage in the male
reproductive tract including seminal vesicles, prostrate or
ejaculatory ducts.
c) Antibody testing:
Doctors are not entirely agreed on the value of antibody testing
for determining infertility. However, if recommended, this
test will be conducted to check for antisperm antibodies in the
blood or seminal secretions.
d) Genetic Test (chromosome
analysis): This test also known as the Karotype test,
examines the chromosomes in your cell for abnormalities that could
interfere with fertility.
e) Testicular Biopsy: This
test is rarely required to aid in determining the possible cause of
male infertility. For this test, a small sample of tissue is
required to be taken from one or both testicles. This
procedure is not usually conducted to detect testicular
cancer.
While most fertility tests for males like physical examination, semen analysis, blood and urine tests are not painful, testicular biopsy could cause a little discomfort. And since fertility tests can be expensive, it is better to discuss with your partner about how far both of you are willing to investigate your possible causes of infertility before embarking on the investigations.
The testicles, also known as the testes, are part of the male reproductive system. Their function is to produce the male gamete spermatozoa, commonly known as sperm. They are also responsible for producing male hormones, most notably testosterone. Healthy and normal functioning of the testicles is, therefore, vital to a high level of male fertility. Many factors can affect the performance of the testicles in producing sperm. This article concentrates on the impact of testicular cancer on male fertility.
Testicular cancer is a rare disease and yet it is the second most common form of cancer affecting males in the age range 18 to 40, with the peak age group for new cases of the disease occurring to men in their thirties. These age ranges also reflect the time when many men will be considering starting a family with their partner, meaning fertility issues could be particularly sensitive to a sufferer of testicular cancer. Testicular cancer is known to be more prevalent in white males than in black and Asian males.
The cause of testicular cancer is generally unknown. There are certain risk factors that are known to contribute to an increased risk of the disease. One of these causes is male infertility itself. This, in turn, could be caused by undescended testicles (Cryptorchidism) or a history of male infertility. Testicular cancer can in itself be a cause of low sperm count in a man. Following successful treatment for testicular cancer, sperm count figures can improve.
In the last 20 years the incidence of testicular cancer has risen in both the USA (4.3%) andUK (3.4%). However, due to advances in medical treatments for the disease the resulting mortality rates have fallen. The survival rate one year after diagnoses is now 97.7% and five years after diagnoses it is above 95%. Treatments include chemotherapy and low-dose radiation therapy. For some individuals testicular cancer may result in radical surgery where the removal of one, or both, of the testicles may be necessary. It is not common for both testes to be found to have cancerous cells, so treatment of both testes is rare. The removal of a single testis (orchidectomy) will not hinder a man’s fertility or sexual performance
Following chemotherapy for testicular cancer most men undergo a temporary period of infertility. In seventy to eighty percent of men, fertility is restored in three to five years following the end of the chemotherapy regime. However, some men do become infertile after chemotherapy. Prior to entering in to a programme of chemotherapy for testicular cancer, men should discuss with their medical advisers the fertility issues that may arise and consider having a sample of sperm and semen frozen for future use.
Where radiation therapy is required the ‘healthy’ testis will be shielded from the effects of the radiation. However, following successful radiation treatment for testicular cancer contraception should be used during any sexual intercourse for two years to avoid impregnation. This is important because the radiation from the therapy can damage germ cell precursors that develop in the sperm. (Germ cell precursors are genes concerned with tissue and organ development. i.e. the radiation therapy could cause genetic damage) It is, again, highly recommended that men entering into a course of radiation therapy discuss with their medical advisers fertility issues and having a sample of their sperm and semen frozen for future use.
Sometimes, the development of testicular cancer requires an operation to remove lymph nodes located at the rear of the abdomen. This is called retroperitoneal lymph node dissection. This operation can be required if, after a course of chemotherapy or radiation treatment, the lymph nodes are still enlarged. Whilst new surgical techniques are reducing the possibility it can unfortunately result in infertility due to retrograde ejaculation. This means that the ejaculation reverses its route into the bladder rather than outward through the penis.
Doctors can prescribe drugs to treat this condition. However, the drugs do carry risks to the heart and blood-pressure and so may not be suitable to all men. There is also is a procedure whereby sperm can be extracted from urine in the bladder following a retrograde ejaculation. The sperm could then be used for artificial insemination. In case retrograde ejaculation cannot be reversed the freezing of sperm and semen samples should be considered with your medical experts.
The prostate gland is one of the
fluid producing organs in the male body. Its function is to produce
seminal fluid (semen) that nourishes and transports the male gamete
(sperm) through the female reproductive tract. Thus its proper and
successful functioning is a key factor in male
fertility.
A healthy prostate gland is made up of
many small fluid producing sacs that are also referred to as
glands. The prostate also contains a network of pipes and muscular
cells that pump the seminal fluid, along with the sperm, at the
moment of a males ejaculation.
The prostate is dormant up to the
point of male puberty. With the release of male hormones it grows
and develops into a walnut/strawberry size, spongy and fluid filled
organ sited beneath the bladder. Its lifelong task is to produce
semen, the complex fluid containing proteins and minerals to
protect sperm as they seek the female gamete, the ovum. (NB. The
prostate also works in conjunction with the seminal vesicles and
Cowper’s gland which also produce fluids that assist
ejaculation.)
Following puberty the size of a healthy prostate will change very little. Apart from a possible episode of inflammation or infection of the prostate most men are completely unconscious of the glands work. At some point, usually in the man’s fifth decade, the prostate will begin to grow again. It can then develop into an intrusive problem affecting the quality of life. The prostate gland is situated in a male’s body in such a position that it can also be seriously affected by problems in another organ. The prostate is inter-connected with the seminal vesicles, the Cowper’s glands, the vas deferens and the urethra. It is also in close proximity to both the bladder and the rectum.
As such it is susceptible to problems developing in other those other sexual, urinary and bowel organs, Begnign Prostatic Hyperlasia (BPH) is a common occurrence in men over the age of 50. In short BPH is the growth of new, non-cancerous, cells in the prostate whilst old cells fail to ‘die’ off. This results in the prostate enlarging and can lead to an abnormally large prostate gland. BPH often results in urinary disorders but rarely causes problems with male fertility.
One of the secretions from the prostate is the protein PSA (prostate-specific antigen). PSA plays the vital role of liquefying coagulated semen so that the sperm are able to ‘swim’ in order to find the ovum. Abnormally high levels of PSA can indicate problems with the functioning of the prostate gland, this could be due to BPH, as described above, or the onset of cancerous cells/growth within the prostate. If cancerous cells are present a variety of treatment options may be available to the medical practitioner. A highly successful treatment for prostate cancer is radiation therapy.
During the 1960’s prostate cancer sufferers undergoing radiation therapy invariably reported sexual dysfunction following it. Modern advances in radiation surgery during the treatment of prostate problems means that this is no longer the case. There has been a great reduction in the chances of sexual dysfunction or side effects arising from radiation therapy prostate cancer treatments. Also, there are now effective therapies to alleviate and even reverse problems that occur after treatment. In summary, most prostate cancer patients can look forward to resuming an active, fertile and fulfilling sexual life after successful treatment.

January 2005 saw the birth of a baby daughter to a Romanian woman, Adriana Iliescu. Possibly an unremarkable event other than at the time of the birth the mother, Adriana, was 66years old. Eliza Maria Iliescu was born six weeks prematurely by caesarean section and weighed 3lbs at birth.
In western cultures there is an increasing trend towards women having their babies in their thirties, whereas previously the dominant trend was to have babies in their twenties. Generally women in their thirties and forties have the fastest rising birth rates. In the USA last year over 9% of births were to women over 40 years of age. Regardless of medical advice, women are increasingly opting to have their children when it fits in with their career, lifestyle and plans. Unfortunately their biological clock will not synchronize itself with their lifestyle and so, in turn,this leads to many of those same women looking to their medical advisors for help in order to conceive a child.
Society in general does not perceive anything wrong or odd for a woman over 40 years of age to be pregnant or even seeking to become pregnant. Media comments about women over 40 becoming pregnant currently seem to centre on those that are post-menopausal. However, is even this worthy of comment? Rather than these older women being seen as ‘going against the natural order’ is it that human and scientific development is outstripping Mother Nature? It’s not that long ago that a woman’s life expectancy would only extend a few years beyond her menopause. Improved medicine, diet, hygiene … etc all mean that compared to the past, women now live well beyond their menopause to 80 and beyond ie a woman age 60having a child could reasonably expect to be alive for a further 20 years to care for her offspring.
Despite the abilities of IVF and other assisted reproductive techniques to assist an older woman to conceive, the question also arises as to how well an older woman might cope with the physical strain of pregnancy and the demands of raising a child as she gets older. Adriana is a single mother who continues to work in order to be able to support her child and rejects any criticism that she is too old to care for her. It is her religious conviction that her daughter’s birth was divinely sanctioned and subsequently she will live to care for her child
No rules exist to govern the eligibility for an assisted reproductive procedure. With the womb transplants undergoing development and tests, women will be able to turn back their biological clock. Medical experts will take into account the welfare of the child, but for a multi-billion dollar international business, it is impossible to set boundaries. There are limits to which biology and biological clocks can be tweaked, other than that the only boundary is one of cost. Basically it comes down to - can the woman cope (psychologically as well as physically) with apregnancy and can she pay!
Risks to women who become pregnant at older and especially post-menopausal ages; over the age of 45 the risk of having a stillbirth doubles, over the age of 45 the risk of having a miscarriage is 50%, if a woman is dependant on donated eggs it can lead to a five-fold increase in the likelihood of developing high blood pressure, beyond the menopause gestational diabetes is 20% more likely to develop and beyond the menopause the risk of pre-enclamsia (rejection of the donated egg as a foreign body) is increased five times. The ‘generation chasm’ is a phenomenon to consider. Can someone who was born during or at the end of the Second World War relate to a child born into the iPod generation? Where will that generation gap be in another 10 years? Being an older parent means an increased risk of mortality prior to the child reaching maturity, this carries a social cost as well as a psychological one for the child. On the other side of the debate is that it’s been found that older parents, having been fully ‘around the block’, tend to be more relaxed about their children’s achievements and potential to succeed. In a recent study the learning scores of children with older parents were found to be higher than those of their peers with youngerparents.
The following article sets out to deliver facts regarding the impact of an abortion on the future fertility of a woman. Whilst abortion is anathema too many it is also for some a physiological and possibly even a psychological necessity. Regardless of the circumstances surrounding an abortion, it is likely that many women and couples will want to know if their future fertility will be affected by it. Please note: this article is not concerned with the ethics of any questions surrounding what is commonly referred to as the ‘abortion debate’.
The ‘bottom line’ on this issue is that when an abortion has been conducted; legally, safely, professionally and providing there are no complications arising from it, there is no significant risk to the future fertility of the woman involved. Some studies have shown a small increase in the risk of having a miscarriage or pre-term delivery in a future pregnancy following an abortion. This is usually caused by cervical incompetence (the cervix being unable to close tightly during pregnancy). The risk of cervical incompetence does increase according to the number of abortion procedures undertaken. However, a properly performed abortion will not affect the woman’s fertility.
Despite the claims of some people there is no evidence that an abortion will cause infertility, stillbirths, ectopic pregnancies or birth defects. However, there is a risk of infertility arising from any subsequent infection, especially when the reproductive organs become infected and are not promptly and correctly treated. Infection in the fallopian tubes could lead to scarring and blockage of the tubes. This would mean that the female gamete (ovum) would be prevented from moving into the uterus. The increased incidence of Chlamydia, which is a sexually transmitted bacterial infection, is known to cause fertility issues for women. Undergoing an abortion whilst suffering from the presence of Chlamydia in a woman would increase the risk of a post-abortion infection and, therefore, the risk of infertility. Screening for Chlamydia before an abortion, followed by an appropriate course of antibiotics will reduce the associated risks
After an abortion a routine ‘check-up’ by your doctor is usually carried out after a couple of weeks. At this the doctor will check for any post-abortion complications. Obviously, following an abortion, if the woman feels uncomfortable about any aspect of her health she should contact her doctor immediately.
Following an abortion, experts now no longer consider it necessary for a woman to undergo a few menstrual cycles before trying to conceive. For a woman who uses a chemical form of contraception after an abortion there is no reason why her fertility should not return to normal as soon as that contraception ceases. Of course, some chemical forms of contraception can take a while for their effects to wear off.
The main risks during an abortion
are; haemorrhaging (heavy bleeding) occuring in 1 in 1000
abortions, cervical damage occurring in up to 10 in 1000 abortions
and womb damage. Womb damage occurs in up to 4 in 1000
abortions, but it falls to 1 in 1000 for mid-trimester
abortions.
To say there are no risks involved
with fertility following an abortion would obviously be false.
However, the few risks that there are must be considered along with
the risks to a woman of continuing with an unwanted pregnancy or
one that is dangerous to her health. Only the woman concerned can
assess the risks and reach for herself a balanced
conclusion.
Many couples who wish to have a baby but are finding it difficult or impossible to do so using their own sperm or eggs can now realize their dream by using sperm or eggs donated by someone else. The practice of donating sperm is a fairly simple procedure and has been around for quite some time. More recent though is the practice of donating eggs for use by women who are unable to produce enough healthy eggs of their own.
Egg donation is a complex process and therefore pays well. If you are someone who is considering becoming an egg donor in response to an advertisement or because someone you know has requested you to do so, it is important to learn all you can about the process, and give very serious thought to all that is involved before committing yourself. This article is about suggesting some of the issues you need to consider and be informed about before taking a decision.
Donating your eggs involves surgery, taking hormones and fertility drugs and possibly, putting on weight. But first, you have to be accepted into an egg donation program. All women do not automatically qualify to donate eggs. Different egg donation programs have different requirements of their prospective donors, but certain criteria are standard for all of them and there are certain legal requirements all programs must cater to.
Most programs require you to be between 21 to 35 years of age which is considered to be the peak reproductive period. Also, while at 21 you can legally contract to donate your eggs, 35 has been kept as the upper limit as older women are likely to have abnormal eggs that could prevent conception or lead to birth defects. Also, older women tend not to react favorably to fertility drugs that they need to take before donating their eggs.
You would be required to undergo a
number of medical tests before being accepted into the
program. These tests would include a physical and
gynecological examination, and blood and urine tests to detect any
existing health problems. Genetic tests as also your medical
and family history would be required to rule out the possibility of
passing on hereditary/genetic problems. You would be asked
about addictions with regard to tobacco, alcohol and prescription
or illegal drugs.
Although genetic tests involve a
simple blood test, the results could impact your ability to get
medical insurance in the future. So you need to check whether
they will provide or refer you to a genetic counselor and if and to
who exactly the program will make your test results
available.
Besides these tests, you will also have to undergo psychological evaluation. Donating your eggs is no simple matter. It involves complex emotional, ethical and social issues that you need to look at and come to terms with before going ahead. This is necessary so as to ensure your ability to fulfill the on complex process involved in donating your eggs as also, to avoid any post donation regrets or emotional trauma. Remember, once you donate your eggs, you have no control over their fate, only the recipient does. She will be the legal birth mother although the baby is genetically related to you.
If you are an ‘anonymous’ donor, some programs may require you to participate in an intelligence test also. The program will attempt to match you to a recipient who has similar physical and mental attributes as you do.
Egg donation requires you to dedicate time for the process, and it does take time. You will need to take medication for around three weeks and make several visits to the program for various tests. This could interfere with your daily routine, your work and your family responsibilities. You would need to make suitable arrangements to allow you to proceed with the program.
You will need to make some lifestyle changes. Drinking alcohol, smoking or taking illegal drugs will not be permissible. You will have to consult and get permission from relevant program authorities before taking prescription or non-prescription medication and you will have to abstain from unprotected sexual intercourse during specific periods of the donation program.
Some programs require their donors to commit to donate eggs several times, before accepting them for the program. Although there is no fixed limit to the number of times you can donate eggs, you need to be careful before agreeing. Firstly, because your eggs could be used to create a number of genetic half-siblings that could possibly end up relating to each other giving rise to a whole host of ethical and other problems. Secondly, since you don’t know how you are going to react to the medications or the procedures you need to undergo for the donating process, it may be a little premature to agree to donate a number of times.
Take time to study all aspects of the egg donation process, get fully informed, get counseled, look at the long term before going forward.
Most people take fertility for granted. Couples imagine that getting pregnant is simple and often put a lot of effort into trying to avoid that very eventuality. Becoming pregnant is not really that easy, even for couples who do not have fertility problems.
Fertility has been studied and
researched in great depth and a fact not many are aware of, is that
humans are one of the least fertile creatures on the planet.
Because conception is possible only during a fairly short period
within the menstrual cycle, the chances of successfully conceiving
is only around 25% each month even among ‘fertile’ couples. And
there are so many other factors also involved in successfully
conceiving - age, health, medical conditions, lifestyle and
timing. Yes, that’s correct; the time has to be
right.
So, how does timing matter?
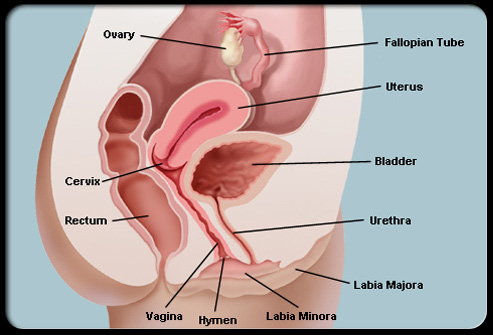
A menstrual cycle is normally between 28 – 32 days and there are two parts to the cycle, pre-ovulation and post-ovulation. Day 1 is the first day of your menstruation. Day 7 is around when your egg is getting ready for fertilization. Based on a 28 day cycle, somewhere between days 11 – 21 are when the egg gets released and moves through the fallopian tubes and towards the uterus. The process where hormones cause the egg to get released from the ovary is known as ovulation. This is when the egg is ready to be fertilized. (It is important to realize that the pre-ovulation period differs in individual cases and can change from month to month, whereas the post-ovulation process is more or less the same for all women.) The gap from ovulation to the next period is normally around 14 days. This gap is used to track and narrow down a woman’s most fertile time in the month.
Once released, while the egg stays around for between 12 to 24 hours before disintegrating, the sperm can survive for up to 72 hours in healthy cervical mucous. It is during this time that the sperm meets up with the egg, penetrates it and the now, fertilized egg fuses with the uterus lining and starts growing.
Getting the time right.
It can be quite challenging to pinpoint exactly when ovulation is going to take place. There are a few ways to achieve this. The easiest but not always accurate method is to keep track of the woman’s menstrual cycle by using one of the following:
• Calendar Tracking Method -
The history of past menstrual cycles is taken as a guide to
estimate the most fertile time in the woman’s cycle. This
method requires you to track your menstrual cycle for 8 – 10 months
and to work out your own ‘fertility window’ which is the time when
you are most likely to get pregnant.
• Basal Body Temperature Method -
Your basal body temperature registers a change post-ovulation and
remains elevated until your next menstrual period.
Monitoring your temperature using a Basal Thermometer over a few
cycles begins to show a pattern that allows you to anticipate when
you are most likely to be ovulating. It is important
that you take your temperature first thing in the morning, before
your active day starts. Ill health, lack of sleep or alcohol
or drug abuse can impact your temperature and disturb the charting
of your basal temperature.
• Cervical Mucus Method - In this
method the consistency of the cervical mucus is studied through the
menstrual cycle. Normally, following a 5 day menstruation
period, there are 3-4 dry days. The wetness of the mucus
increases daily thereafter until it reaches its wettest condition
when it becomes abundant, clear and stretchy. This condition
is reached when you are ovulating. Remember that the use of
spermicides and douches during this period impacts the consistency
of the mucus thus nullifying the possibility of examining
it.
These methods can achieve up to 90%
accuracy if used correctly for women who have fairly regular
cycles. They can be a bit of a challenge for those with
irregular cycles though.